Overview
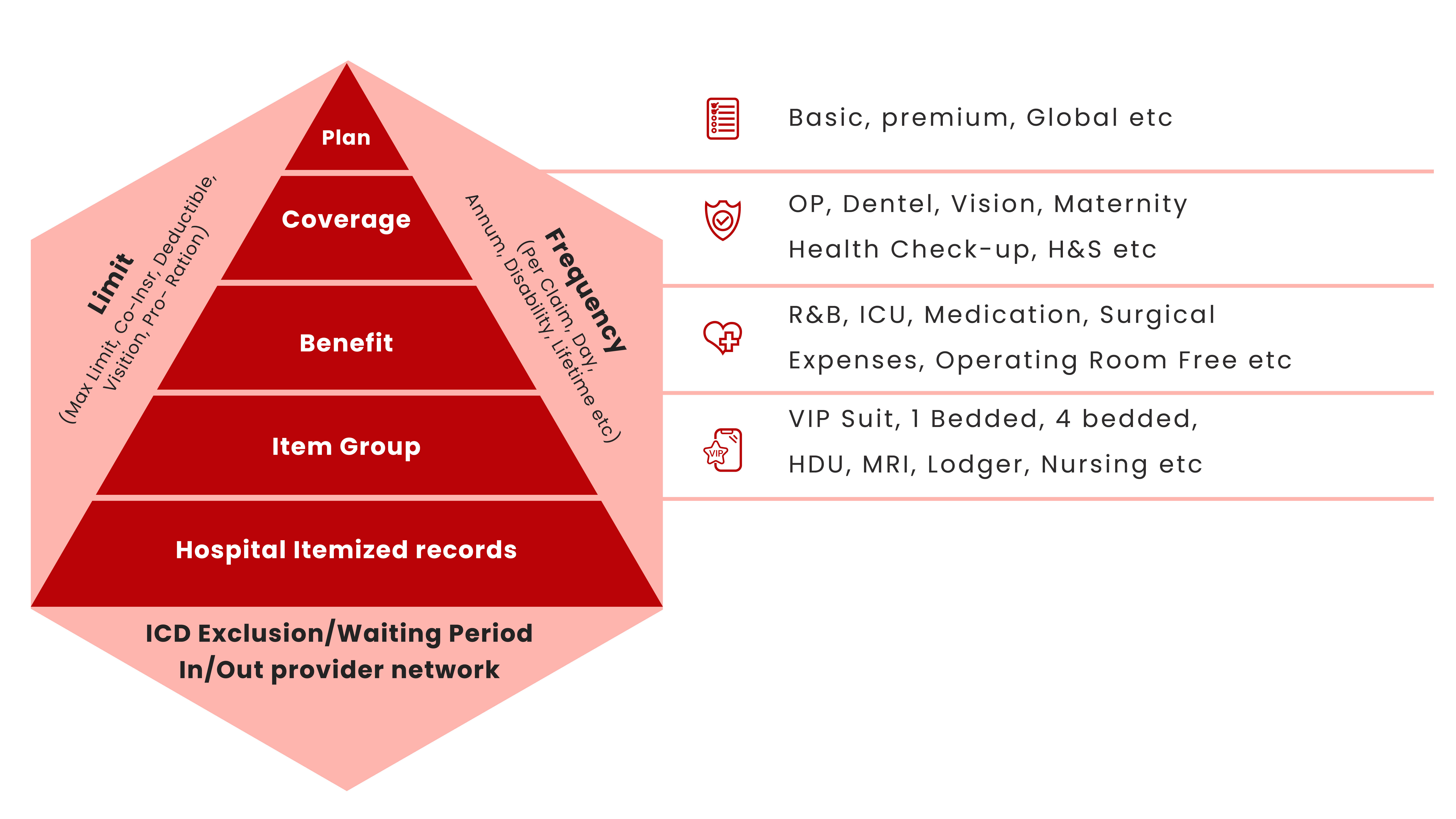
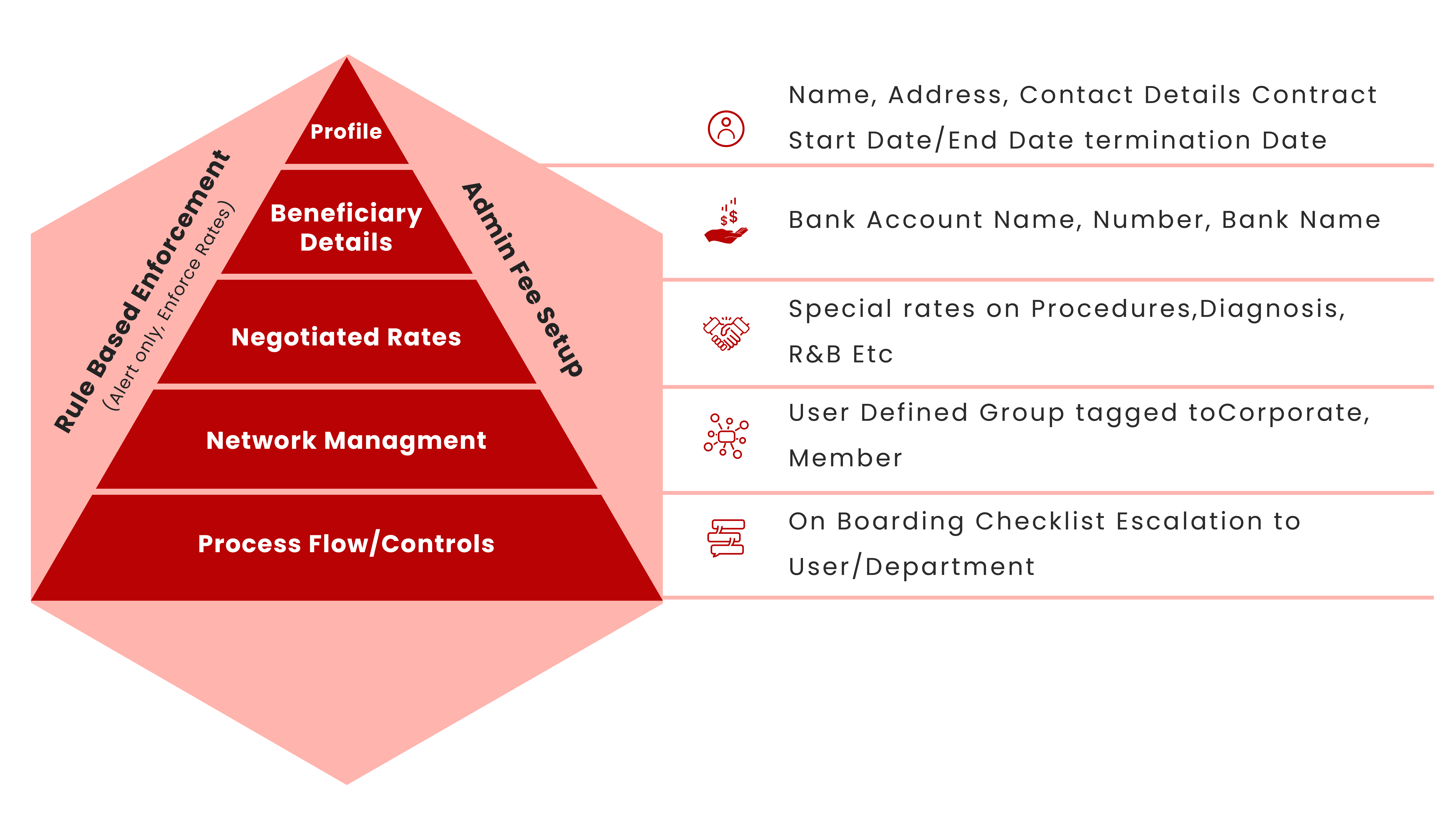
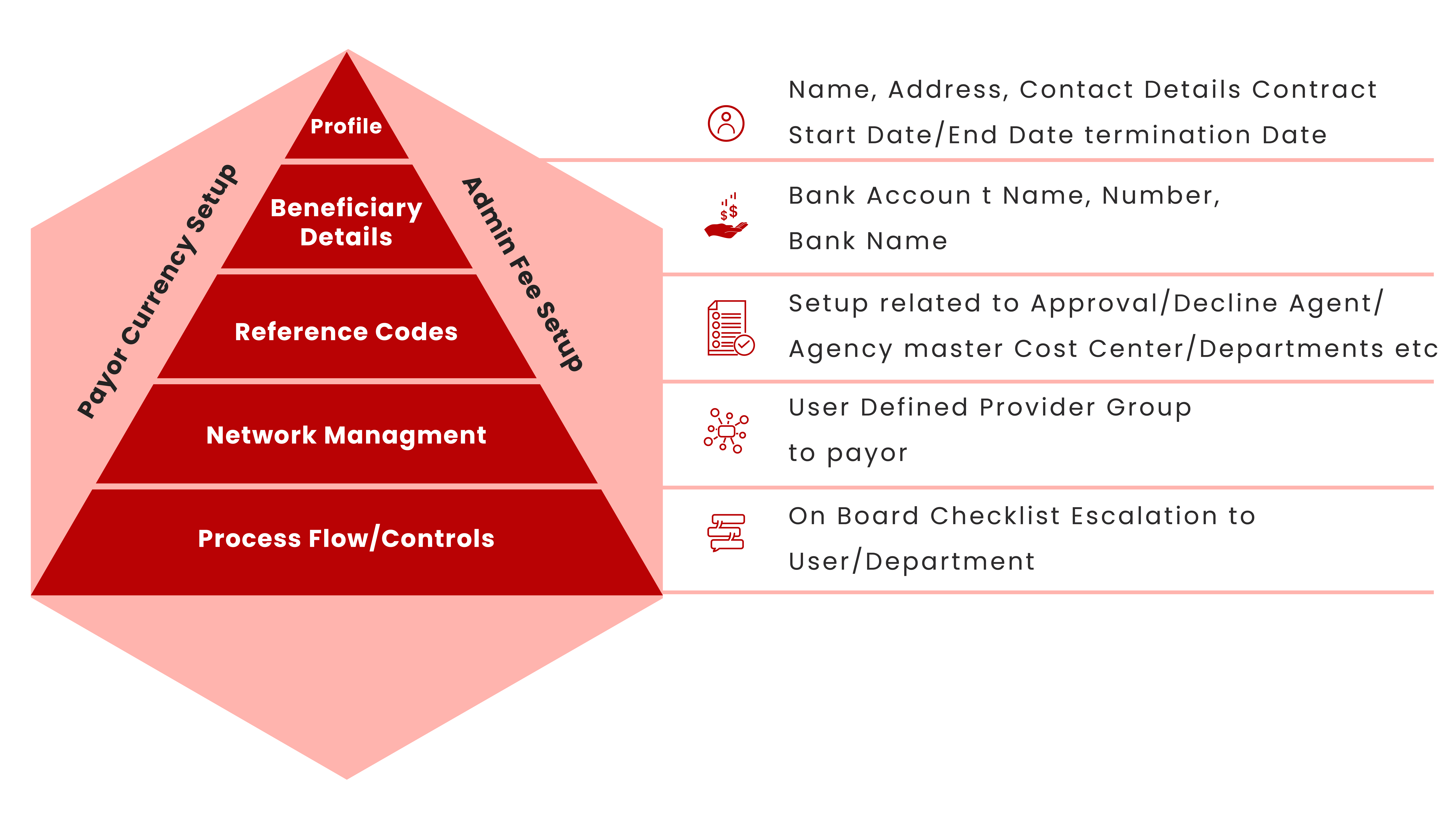
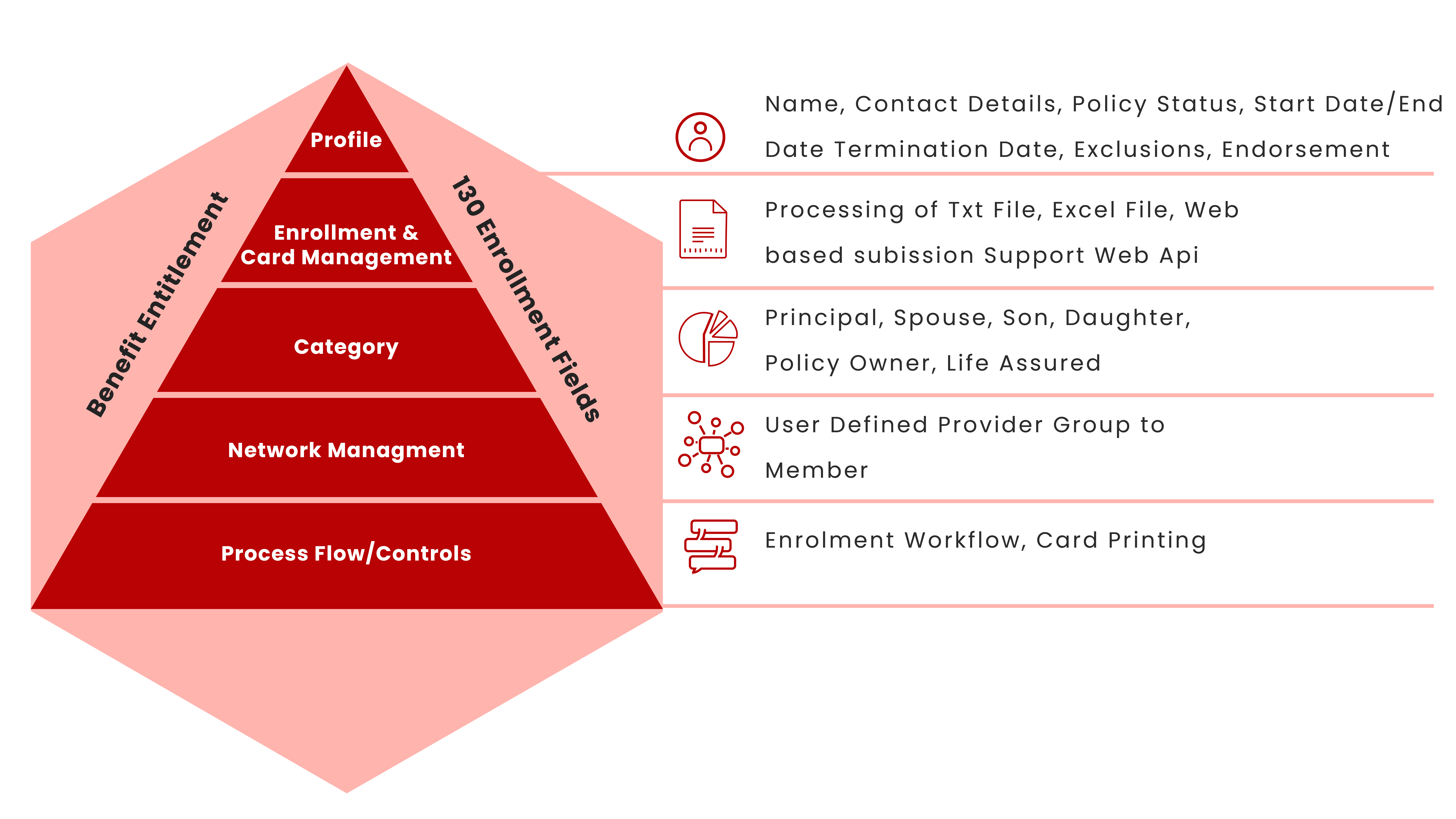
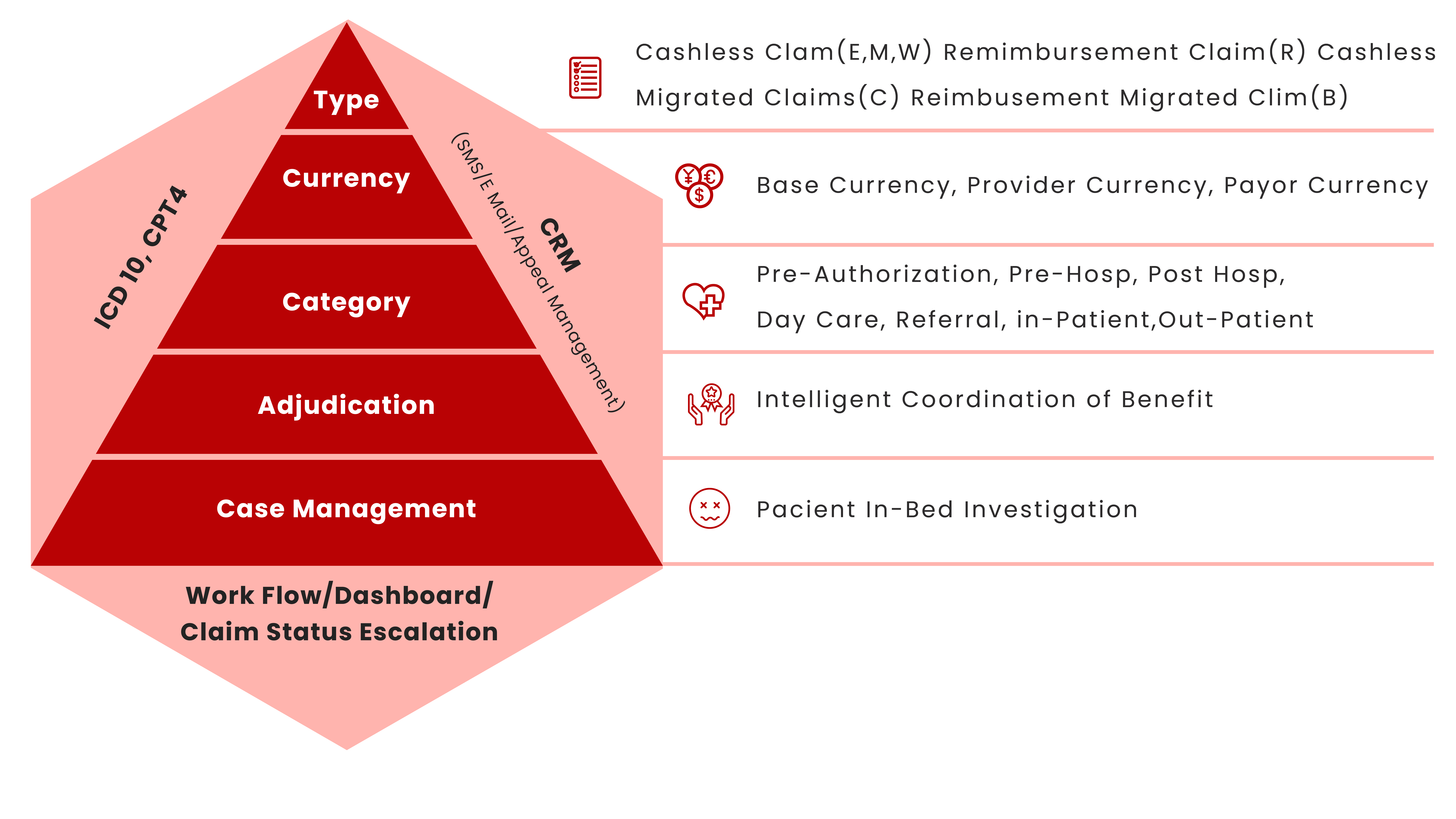
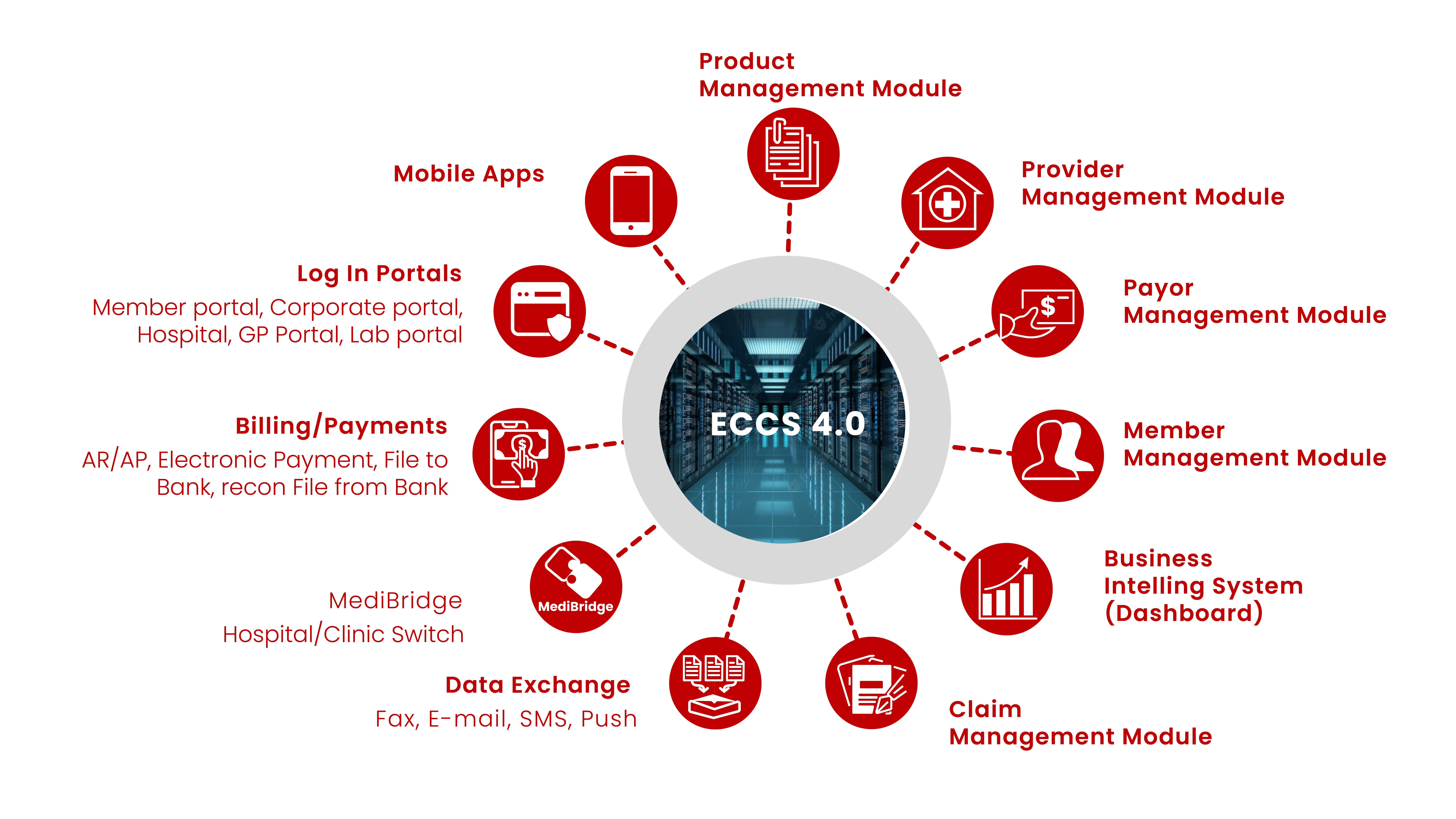
The Medilink-Global’s Claims Management System (ECCS) 4.0, which runs on the Oracle Database platform, is a complete suite of highly customized system designed for healthcare claims processing and healthcare data management. The software manages various databases pertaining to the Healthcare Payor and its members, their Health Plans, Benefits, Coverage, Exclusions, Specified Conditions and Conditions.
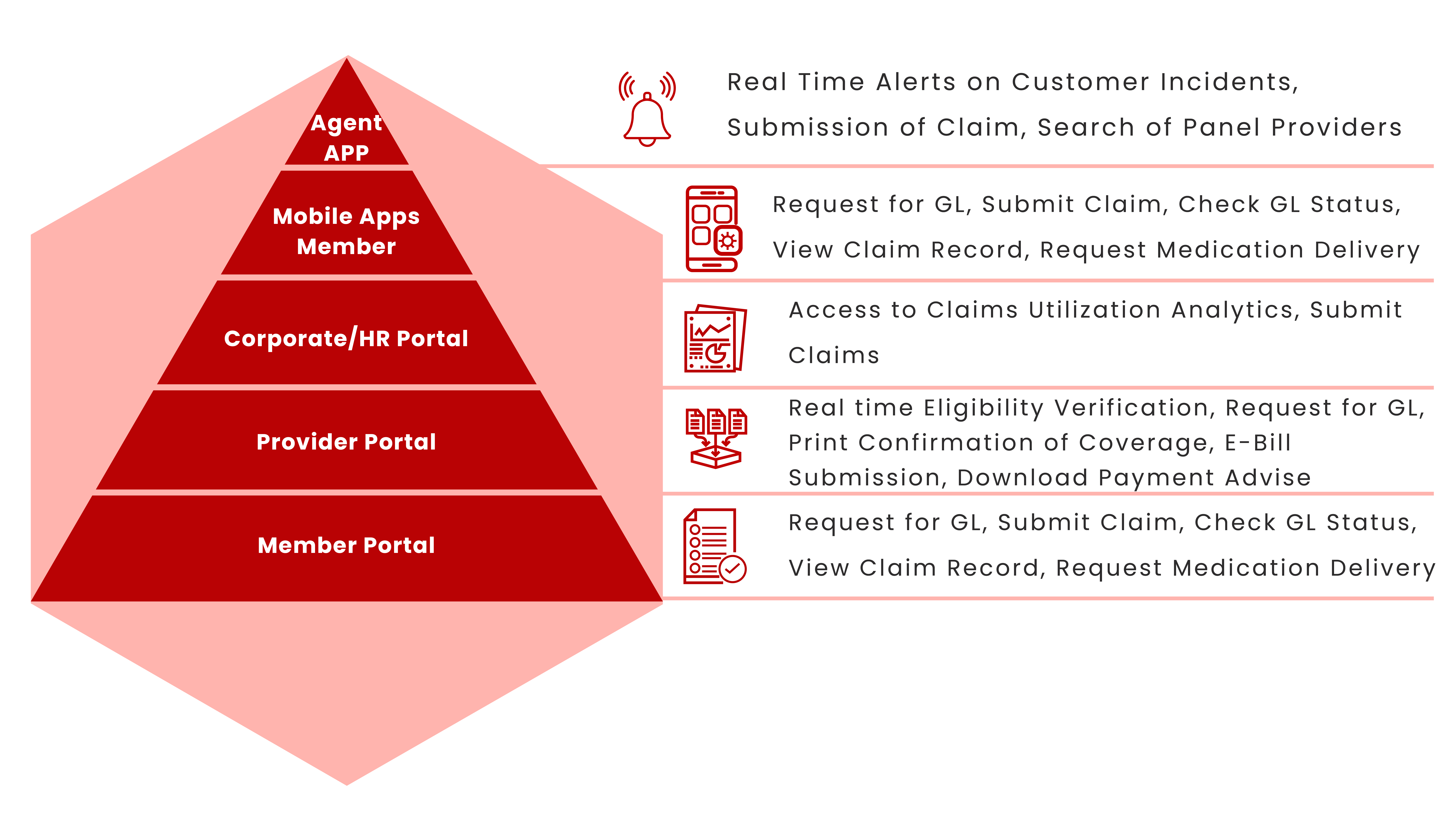
The versatile and highly customizable Application Software would empower Claims Administration Team of Insurance Companies, TPA Providers or Self-insured corporations to manage claims for almost limitless variety of benefit designs of healthcare schemes.
The wealth of data generated by the System supplies vital information for the Insurance Companies, TPA Providers or Self- insured corporations to manage their claims in an efficient and effective manner in order to ensure the long-term viability of the schemes.
The update of policy holder's status in ECCS has to be done via electronic file, generated from other existing sub-system of the Insurance Company, TPA Provider or Self- insured Corporation. All data submitted to the system is subject to programmed validation using highly stringent criteria for data integrity checking.
The system also manages the claims database to monitor the utilization trend, medical history and current eligible balances of each policyholder. The medical related data is managed with the highest standard of security, privacy and confidentiality.
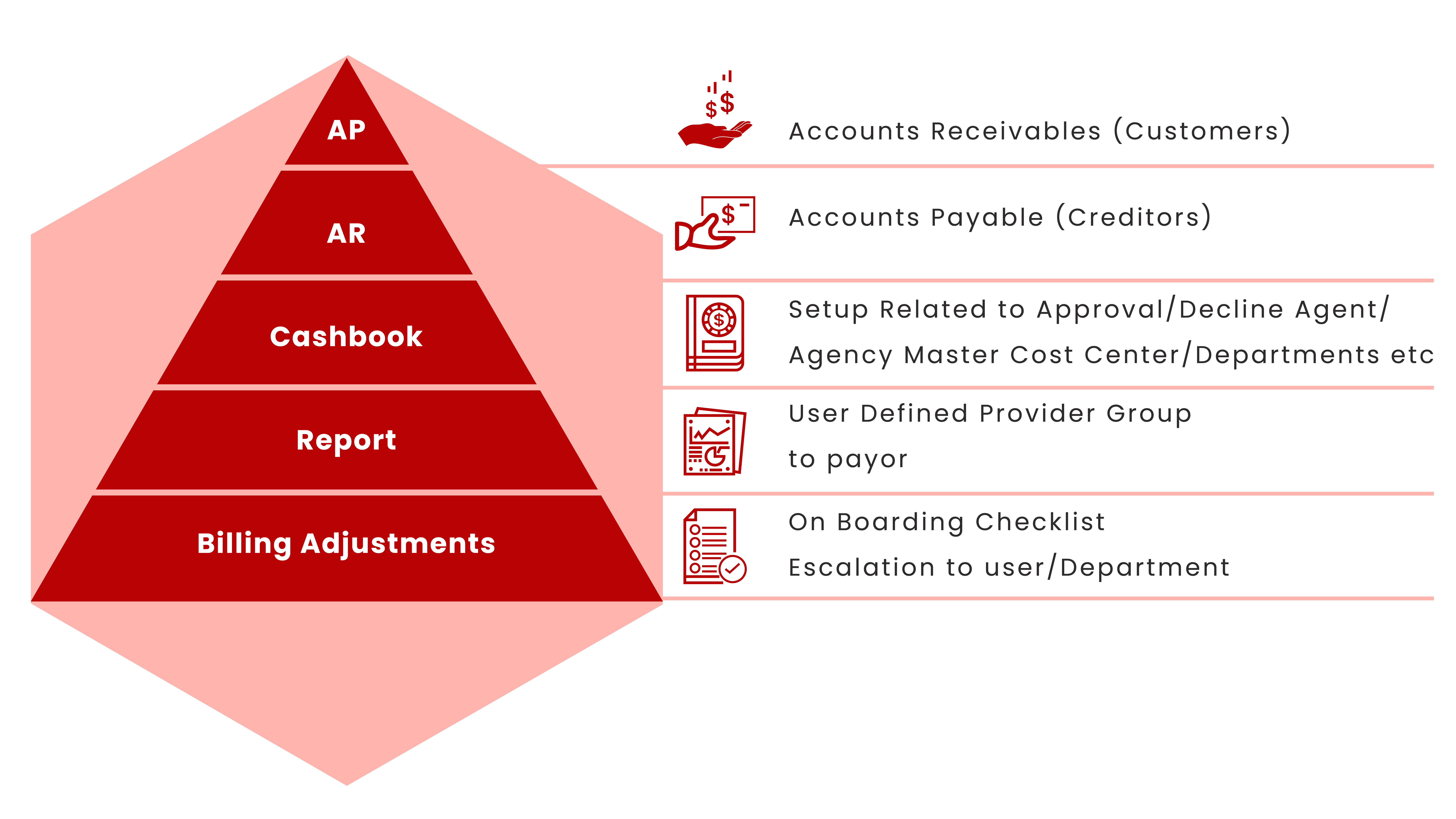
By virtue of its design, the system could generate a comprehensive set of reports for claims management review, healthcare analysis, underwriting, financial planning and healthcare risk management.
- Supports Medilink’s TPA operations in Malaysia, Singapore, China and its business partner in Indonesia
- Serving > 30 Insurance Companies and hundreds of
- Handling variety Health Plans Design
- Processed >15,000,000 Out Patient and In-Patient Claims since year 2011
Major Modules